Ankylosing spondylitis (AS) is a kind of inflammatory arthritis that mostly affects the spine. It can severely restrict movement. Treatment of AS includes a variety of approaches, but one of the most significant is regular exercise.
This article looks at the potential contributions a physical therapist could make in the life of someone with AS.
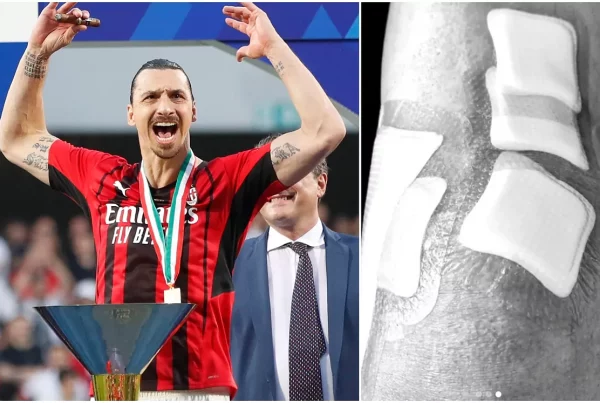
What Is Ankylosing Spondylitis?
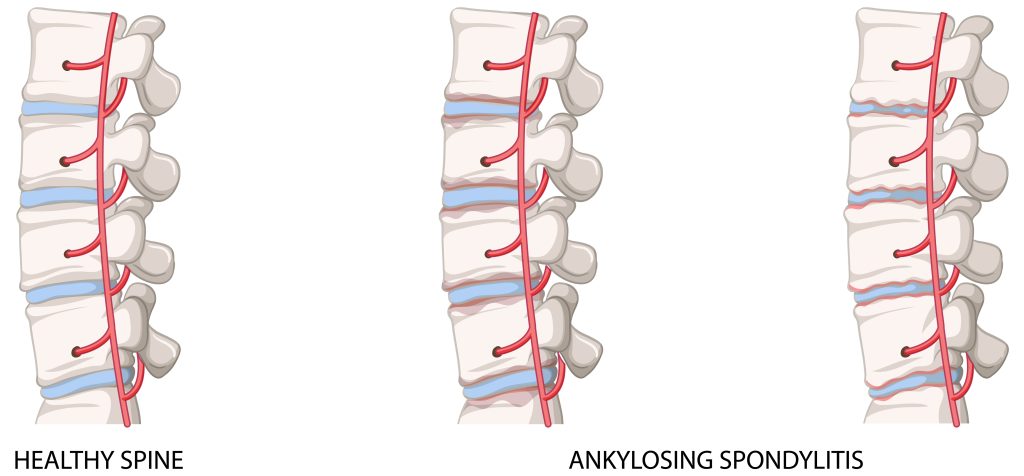
Ankylosing spondylitis involves inflammation. However, AS is a lifetime condition. Inflammation and stiffness of the ligaments and joints in the back can occur with ankylosing spondylitis.
Spinal fusion is a possible complication. It can make it extremely uncomfortable to move and severely restrict mobility. Joints in the spine and the sacroiliac region may fuse due to abnormal bone growth in AS. Affected individuals may also experience problems with their eyes, ears, and heart.
In general, AS strikes younger adults, which is more common in males than women.
What Causes Ankylosing Spondylitis?
Although the root causes of AS are still unclear, most patients can trace their ailment back to a relative who also suffers from it.
HLA-B27 is one of several antigens that have a link to AS. However, not everyone who has the HLA-B27 antigen will develop AS. HLA-B27 antigen may aid germs in attacking the host, leading to AS, according to research.

The most prevalent triggers for ankylosing spondylitis are:
- Someone in your family has been diagnosed with AS
- Having the HLA-B27 antigen present
- Differences in sex and old age
How Does It Feel?
Some of the earliest warning signs of ankylosing spondylitis include:
- lower back and hip discomfort, especially upon rising or after prolonged inactivity
- weakness and neck pain
- morning stiffness or after inactivity which subsides with movement or activity
Other symptoms may include:
- fever
- inflammation
- feeling run down
- losing your appetite
- breathing problems due to stiffening of the lungs and the rib-spine joints
- Conjunctival edema (uveitis)
- Redness, pain, “floaters,” and a heightened sensitivity to light in the eyes
Changes in symptom severity, frequency, or even a complete cessation of symptoms may occur intermittently. The most common areas of impact are:
- The joint at the bottom of the spine where meets the pelvis.
- Lumbar spine vertebrae
- tendon and ligament attachment sites, most commonly along the spine but also the heel bone
- The cartilage that connects the breastbone to the ribs.
- Hip and shoulder articulations
How Is Ankylosing Spondylitis Diagnosed?
Your physical therapist will examine your spine, hips, knees, and shoulders to determine your range of motion. Your PT will carefully evaluate your ability to bend, squat, and walk. In addition, they will feel uncomfortable points in your spine, hips, and sacroiliac joints.
If your PT has reason to suspect AS, they will likely also measure the amount your chest expands during a deep breath and exhale. That will reveal how the AS is influencing your ribs and airflow.
Your physical therapist will assess your fall risk by watching how you walk, get up from sitting, and test your balance.
A physical therapist who believes their patient has AS will work with the patient’s doctor to arrange diagnostic imaging. A positive blood test result can indicate an increased risk of AS for the HLA-B27 gene.
Treatment
The purpose of treatment is to reduce discomfort and stiffness. In addition, aims to prevent further damage to the spine and any potential problems. It is best to treat ankylosing spondylitis early before the condition causes permanent disability.
Medications
Ankylosing spondylitis sometimes gets treated with nonsteroidal anti-inflammatory medicines (NSAIDs) like:
- naproxen (Aleve, Naprosyn, and others)
- ibuprofen (Advil, Motrin IB, and others)
These drugs reduce swelling, discomfort, and stiffness but may induce internal bleeding in certain people.
Physical Therapy
Unfortunately, there is currently no medical solution for AS. Thus physical therapy is the recommended course of action. Seeing a PT can help individuals with AS improve their posture and mobility, lessen pain and suffering, and make it easier to carry out routine tasks.
Posture Training
Good posture strategies assist you in avoiding slouching forward, reducing the pressure on your spine.
- Back against a wall
- Position yourself on your stomach on a flat, hard surface.
- Support your body with a cushion or cloth under your chest or forehead.
- Bring your arms to your sides and straighten them.
- Train yourself to stay like that for 20 minutes.
- Prone lying
- Position yourself against a wall, so your heels, butt, and shoulders touch it.
- Put the head back up against the wall.
- Rest and repeat the posture after a brief hold.
Deep Breathing Exercises
Expanding your chest will improve your ability to breathe.
- To begin, choose a comfortable position and take a deep, steady breath. Relax your abdominal muscles and let your lungs fill up completely.
Exhale completely and notice how your belly button drops as you do so. - Repeatedly switch between shallow and deep breathing.
Stretching Exercise
You can lower the risk of joint fusion, and mobility and flexibility increase with regular stretching.
- Seated Thoracic Extension
- Place your feet flat on the floor and sit straight on a chair.
- For further support, try resting your hands behind your head while keeping your elbows by your sides.
- Keep your head steady as you slowly move your upper back over the chair’s back.
- Keep this position for 5–10 seconds, then release and return to the starting position.
- Repeat
- Quadriceps
- Make yourself comfortable by lying on your stomach.
- Wrap a belt or sheet over your foot and secure it with a buckle.
- Carefully raise the strap until you feel a slight tension in the shoulder muscle.
- Hold for 10 to 20 seconds, then return to the starting position.
- Repeat on the opposite side.
- Seated Figure of Four Stretch
- Put your feet flat on the floor and sit straight on a chair.
- Put the sole of your right foot on top of your left thigh, above the knee. Then, raise your right leg.
- Slowly bend forward while maintaining a completely straight spine.
- Gently squeeze on the right thigh to increase the depth of the stretch.
- Hold for 10 to 20 seconds before returning to the starting position.
- Repeat on the opposite side.
- Plank
- Get down on your belly, elbows under your shoulders, and place your forearms on the floor.
- Lift your hips off the ground and contract your abs to achieve this position.
- Contract your buttocks and lift your knees off the floor.
- Don’t slouch or allow your pelvis to drop to the floor; keep your body rigid.
- Hold for 10 to 20 seconds before returning to the starting position.
- Repeat.
Strengthening Exercises
Lifting dumbbells or weights or working against resistance during strength training helps build muscular strength. People with AS should strengthen their core muscles to stabilize their spine better. Those who regularly exercise their abs and pelvic floor typically have reduced back discomfort.
Aquatic Exercises
As a result of the buoyancy of the water, water aerobics can reduce joint discomfort and increase flexibility.

Flexibility Exercises

Gentle range-of-motion and stretching exercises keep the spine and other joints flexible and prevent stiffness.
Lifestyle and Home Remedies
Ankylosing spondylitis can be dealt with by lifestyle.
- Stay Active. Exercise reduces pain, improves flexibility, and corrects posture.
- Quit smoking. Smoking is terrible for overall health. It causes particular concerns for persons with ankylosing spondylitis, including respiratory difficulty.
- Use proper posture. Standing upright in front of a mirror might assist with ankylosing spondylitis.
A Note From Gulf Physio
We hope you’ve enjoyed learning about the subject matter above. This blog post is not a substitute for medical advice. The author cannot guarantee the accuracy of the information presented. If you have any questions or concerns, please consult a healthcare professional. All decisions and actions you make are your own. No one involved in making this resource is liable for its use.